What does Medicaid cover?

MHD continues to monitor the Centers for Medicare and Medicaid Services (CMS) guidance related to COVID-19 testing and specimen collection. The tables below list the COVID-19 testing and specimen collection procedure codes MO HealthNet currently covers as well as who can bill each code, effective dates, max units, and rates. In all states, Medicaid can be used as a secondary insurance for Medicare recipients. Disabled individuals or seniors who fall within the specified income guidelines can receive help with their deductible and co-pays from Medicaid. Supplemental Security Insurance (SSI) beneficiaries are automatically eligible for Medicaid coverage. Call the Ohio Medicaid Consumer Hotline at (800) 324-8680 if you have more questions. Non-emergency services obtained in a hospital or emergency room. Dental services. Eye examinations. $2 per examination.
Medicaid is a social insurance program administered by state and federal governments designed to cover the basic healthcare needs of lower income families in America. This means that Medicaid helps people with low incomes cover their health care costs. But what does Medicaid cover for you? And are you eligible for Medicaid in your state?
To qualify for Medicaid coverage, a person must make less than 133 percent of the federal poverty line, which is about $16,000 for an individual or about $32,000 for a family of four.
In recent years, Medicaid enrollment has surged across the U.S. and now, along with the companion Children’s Health Insurance Program (CHIP) program, cover more than 74 million people.
Medicaid vs. Medicare: They are not the same
Before understanding what services Medicaid covers, it’s important to clear up any confusion regarding the relationship and the differences between Medicaid and Medicare. Both were created in 1965 in response to the inability of older and low-income Americans to buy private health insurance. Their goal was to allow the financial burdens of illnesses to be shared among sick and healthy people, and affluent and low-income families.
There are clear differences between Medicaid and Medicare, although many people may be eligible for both programs.
Medicaid is a state and federal program that provides health coverage if you have a very low income.
Medicare is a federal program that provides health coverage if you are 65 or older or have a severe disability, no matter what your level of income is.
Medicaid is jointly funded by the federal government and state governments. It is administered by state governments, and each one has broad leeway in determining how Medicaid is implemented. To be reimbursed by the federal government, there are certain mandatory Medicaid benefits that states much offer qualified participants.
For example, if you live in Texas, the federal government requires that inpatient and outpatient hospital services must be covered, among many other mandatory benefits. However, coverage for other services that are considered optional will vary depending on one of the four particulars plan that you decide to enroll in.
And, if you live in New York, you will be covered for all required federal benefits. However, you may have to pay a small co-pay for other benefits such as certain lab tests, medical supplies and emergency room visits.
Mandatory Medicaid benefits
States are required to provide the following mandatory Medicaid benefits under federal law.
- Inpatient hospital services
- Outpatient hospital services
- EPSDT: Early and Periodic Screening, Diagnostic and Treatment Services
- Nursing facility Services
- Home health services
- Physician services
- Rural health clinic services
- Federally qualified health center services
- Laboratory and X-ray services
- Family planning services
- Nurse midwife services
- Certified pediatric and nurse practitioner services
- Freestanding birth center services (when licensed or otherwise recognized by the state)
- Transportation to medical care
- Tobacco cessation counseling for pregnant women
Optional Medicaid benefits
Medicaid also covers many optional services as well. States may choose to provide the following optional Medicaid services at their discretion:
- Prescription drugs
- Clinic services
- Occupational therapy
- Speech, hearing and language disorder services
- Respiratory care services
- Other diagnostic, screening and rehabilitative services
- Podiatry services
- Optometry services
- Medicaid dental coverage
- Dentures
- Prosthetics
- Eyeglasses
- Chiropractic services
- Other practitioner services
- Private duty nursing services
- Personal care
- Hospice
- Case management
- Services for individuals age 65 or older in an institution for mental disease
- Services for an intermediate care facility for individuals with intellectual disability
- State Plan Home and Community Based Services – 1915 (i)
- Self-directed Personal Assistance Services – 1915 (j)
- Community First Choice Option – 1915 (k)
- TB Related services
- Inpatient psychiatric services for individuals under age 21
- Other services approved by the Secretary including services furnished in a religious nonmedical health care institution, emergency hospital services by a non-Medicare certified hospital, and critical access hospital (CAH).
- Health Homes for Enrollees with Chronic Conditions – Section 1945
Each state provides a combination of these optional services. More than likely, your state does not provide coverage for all the optional services, but it is important to check prior to seeking help, so you know financially what you will be responsible for.
Some states choose to offer optional benefits but at a limited cost to the customer, so Medicaid recipients may be expected to pay a co-payment or pay a portion of the total cost. For example, when it comes to prescription drug coverage, states are allowed to offer coverage for generic versions of medicines as a way of encouraging patients to choose generic options over their more expensive counterparts.
What does Medicaid cover in your state
To give you a better idea of how wide the range of services can be from state to state, here’s a comparison of optional benefits for Medicaid coverage in four states:
Medicaid Coverage in Nevada (NV)
What does Medicaid cover in Nevada?
Nevada Medicaid provides quality health services to low-income Nevadans who qualify based on state and federal law. Nevada Medicaid does not reimburse an individual for medical services. Payments are sent directly to health care providers when they render services to Medicaid recipients.
Nevada Check Up is offered concurrently with Medicaid and is designed for children who do not qualify for Medicaid but who come from families with incomes that are at or below 200% of the Federal Poverty Level. Nevada Medicaid is the payer of last resort, meaning that if you have other health insurance that can pay a portion of your bills, then payment will be collected from them first. Benefits covered by Nevada Medicaid and Nevada Check Up include:
- Ambulance/Transportation
- Birth Control/Family Planning
- Medicaid Dental Coverage
- Disposable Medical Supplies
- Durable Medical Equipment
- Orthotics & Prosthetics
- Doctor Visits
- Emergency Room
- Eye Exams and Eyeglasses
- Healthy Kids/Early Periodic Screening Diagnosis and Treatment (EPSDT) or Preventive Health Services for Children
- Hearing Tests
- Home Based Habilitation Services (HBHS)
- Home Health Care
- Hospice Care
- Hospital Care
- Immunizations
- Lab and Radiology Services
- Maternity Care
- Mental Health/Substance Abuse Services
- Midwife Services
- Nursing Home Services
- Occupational Therapy Services
- Over-the-Counter Drugs with a Prescription
- Personal Care Services
- Physical Therapy Services
- Preventative Screenings
- Early Periodic Screening and Diagnostic Treatment (EPSDT)/Healthy Kids
- Private Duty Nursing
- Prescription Drugs
- Smoking Cessation Products
- Specialists
- Speech and Hearing Services
- Transportation Services (Non-emergency transportation is not a Nevada Check Up benefit)
- Waiver Program Services (Not a Nevada Check Up benefit)
Medicaid Coverage in Texas (TX)
What does Medicaid cover in Texas?
Texas Health and Human Services administers Medicaid and CHIP in the state. It administers four Medicaid programs: STAR, STAR+PLUS, STAR Health and traditional Medicaid. The type of Medicaid coverage a person gets depends on where the person lives and what kind of health issues the person has.
Traditional Medicaid —Traditional Medicaid is for those who can't be in manage care. Traditional Medicaid is also called fee for service.

STAR — STAR is Medicaid coverage for children, newborns, pregnant women and some families and children. People in STAR get their services through health plans, also called managed care plans.
STAR Kids — STAR Kids is a new Medicaid program for children and adults 20 or younger who have disabilities. Under STAR Kids, you will get basic medical and long-term care services and supports through the health plan's provider network. You also will get Medically Dependent Children Program (MDCP) waiver services through the health plan's provider network, if you are eligible.
STAR+PLUS — STAR+PLUS is a Medicaid program for people who have disabilities or are age 65 or older. People in STAR+PLUS get Medicaid basic medical services and long-term care services through a health plan, also called a managed care plan.
STAR Health is Medicaid coverage for children who get Medicaid coverage through the Texas Department of Family and Protective Services. STAR Health also is for young adults who were previously in foster care and have either: Former Foster Care Children's Medicaid or Medicaid for Transitioning Youth. Young adults who are in the Former Foster Care in Higher Education program also get services through STAR Health.
These benefits include:
- Dentist visits, cleanings, and fillings
- Eye exams and glasses
- Choice of doctors, regular checkups, and office visits
- Prescription drugs and vaccines
- Access to medical specialists and mental health care
- Hospital care and services
- Medical supplies, X-rays, and lab tests
- Treatment of special health needs
- Treatment of pre-existing conditions
Medicaid Coverage in New York (New York State)
What does Medicaid cover in New York?
The New York State Medicaid State Plan is administered by the NY Department of Health.
In general, the following services are paid for by Medicaid, but some may not be covered for you because of your age, financial circumstances, family situation, transfer of resource requirements, or living arrangements.
Some services have small co-payments. These services may be provided using your Medicaid card or through your managed care plan if you are enrolled in managed care. You will not have a co-pay if you are in a managed care plan, except for pharmacy services, where a small co-pay will be applied.
- smoking cessation agents
- treatment and preventive health and dental care (doctors and dentists)
- hospital inpatient and outpatient services
- laboratory and X-ray services
- care in a nursing home
- care through home health agencies and personal care
- treatment in psychiatric hospitals (for persons under 21 or those 65 and older), mental health facilities, and facilities for the mentally retarded or the developmentally disabled
- family planning services
- early periodic screening, diagnosis, and treatment for children under 21 years of age under the Child/Teen Health Program
- medicine, supplies, medical equipment, and appliances (wheelchairs, etc.)
- clinic services
- transportation to medical appointments, including public transportation and car mileage
- emergency ambulance transportation to a hospital
- prenatal care
- some insurance and Medicare premiums
- other health services
- If you are eligible for Medicaid, you will receive a Benefit Identification Card which must be used when you need medical services. There may be limitations on certain services.
- For you to use your Benefit Identification Card for certain medical supplies, equipment, or services (e.g., wheelchair, orthopedic shoes, transportation), you or the person or facility that will provide the service must receive approval before the service can be provided (prior approval).
The following services are subject to a co-payment:
- Clinic Visits (Hospital-Based and Free Standing Article 28 Health Department-certified facilities) - $3.00;
- Laboratory Tests performed by an independent clinical laboratory or any hospital-based/free standing clinic laboratory - $0.50 per procedure;
- Medical Supplies including syringes, bandages, gloves, sterile irrigation solutions, incontinence pads, ostomy bags, heating pads, hearing aid batteries, nutritional supplements, etc. - $1.00 per claim;
- Inpatient Hospital Stays (involving at least one overnight stay; is due upon discharge) - $25.00;
- Emergency Room - for non-urgent or non-emergency services - $3.00 per visit;
- Pharmacy Prescription Drugs - $3.00 Brand Name Non-Preferred, $1.00 Brand Name Preferred, $1.00 Brand When Less Than Generic, $1.00 Generic;
- Non-Prescription (over the counter) Drugs - $0.50.
There is no co-payment on private practicing physician services (including laboratory and/or x-ray services, home health services, personal care services or long term home health care services).
You are responsible to pay a maximum of up to $200 in a co-pay year. Your year begins on April 1st and ends March 31st each year. If you reach your maximum of $200, a letter will be sent to you exempting you from paying Medicaid co-payments until April 1st.
Medicaid Coverage in Pennsylvania (PA)
What does Medicaid cover in Pennsylvania?
In 2015, the State of Pennsylvania revamped its Medicaid program, streamlining coverage and added Medicaid dental coverage and non-emergency transportation to medical appointments. Called the Adult Medicaid Healthy Plus Benefits Package, it replaced the Interim Healthy Benefits Package for most adults. However, many adults still receive benefits under the Interim coverage.
The state currently contracts with ten plans to manage care for beneficiaries, including three national, for profit plans (Aetna Better Health, UnitedHealthcare Community Plan, and Coventry Cares Health Plan), and three national, not-for- profit plans (AmeriHealth Caritas Pennsylvania, AmeriHealth Northeast, and Keystone First).
The state also contracts with three local, not-for-profit plans, (UPMC for You, Health Partners of Philadelphia, and Geisinger), and one local, for profit plan (Gateway Health Plan). The state also contracts with five Behavioral Health Organizations (Magellan Behavioral Health; Community Care Behavioral Health Organization; Community Behavioral Health; PerformCare; and Value Behavioral Health of Pennsylvania) to manage the behavioral health component of HealthChoices.
A few frequently asked questions about what Medicaid covers
What coverage do pregnant women get under Medicaid?
Pregnant women are covered for all care related to the pregnancy, delivery and any complications that may take place during pregnancy and up to 60 days postpartum.
Pregnant women may also qualify for care that was received for their pregnancy before they applied and received Medicaid. Some states call this “Presumptive Eligibility” and it was put in place so that all women would start necessary prenatal care as early in pregnancy as possible. Pregnant women are usually given priority in determining Medicaid eligibility. Most offices try to qualify a pregnant woman within about 2-4 weeks.
Does Medicaid cover VSG?
Vertical sleeve gastrectomy, also known as VSG, is surgery to help with weight loss. Medicaid does not cover weight loss surgery in most cases. However, it is best to check with your state on an individual basis to confirm that they do not offer it as a benefit separate from mandatory federal benefits.
Does Medicaid cover dental services?
Medicaid pays for emergency and medically necessary dental work across the country. Medicaid also pays for comprehensive dental care in more than 30 states. However, others may only cover certain categories of treatments. Medicaid does cover dental services for all child enrollees as part of the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit. Check with your state to see what your exact level of dental coverage is.
What does Medicaid cover for children?

Children’s Medicaid and CHIP offer many benefits, including dental services, eye exams and glasses, regular checkups and office visits, prescription drugs, vaccines, access to medical specialists, mental health care, hospital care, medical supplies, X-rays, lab tests, and treatment of special health needs and pre-existing conditions.
Does Medicaid cover orthotics?
Medicaid does cover for orthotics, but that coverage will vary from state to state. In some instances, if you have Medicare as well, Part B could cover orthotic devices or braces to support weak joints or muscles.
How to apply for Medicaid
Because Medicaid is administered through the state and states determine eligibility, you will need to visit your state's Medicaid office or website to apply. When applying you will need proof of income, residency, age, citizenship and/or immigration status for every member of your household.
Contact your state Medicaid office (see state program information below). Getting approved for Medicaid can take time, so start the application process as soon as there is a clear need. Most offices allow you to apply or at least start your request online. You may need to go into one of their offices for an interview as part of the application process. Have all your needed verification documents ready.
Medicaid’s Eligibility factors include income, residency, age, citizenship, immigration status, household composition, and pregnancy.
The exact verification documents you will need will vary based on what state you are in. However, be prepared to have any proof of income, proof of residency, your social security card, and immigration status confirmation documents on hand (if applicable). Generally, household composition and pregnancy status do not require formal verification.
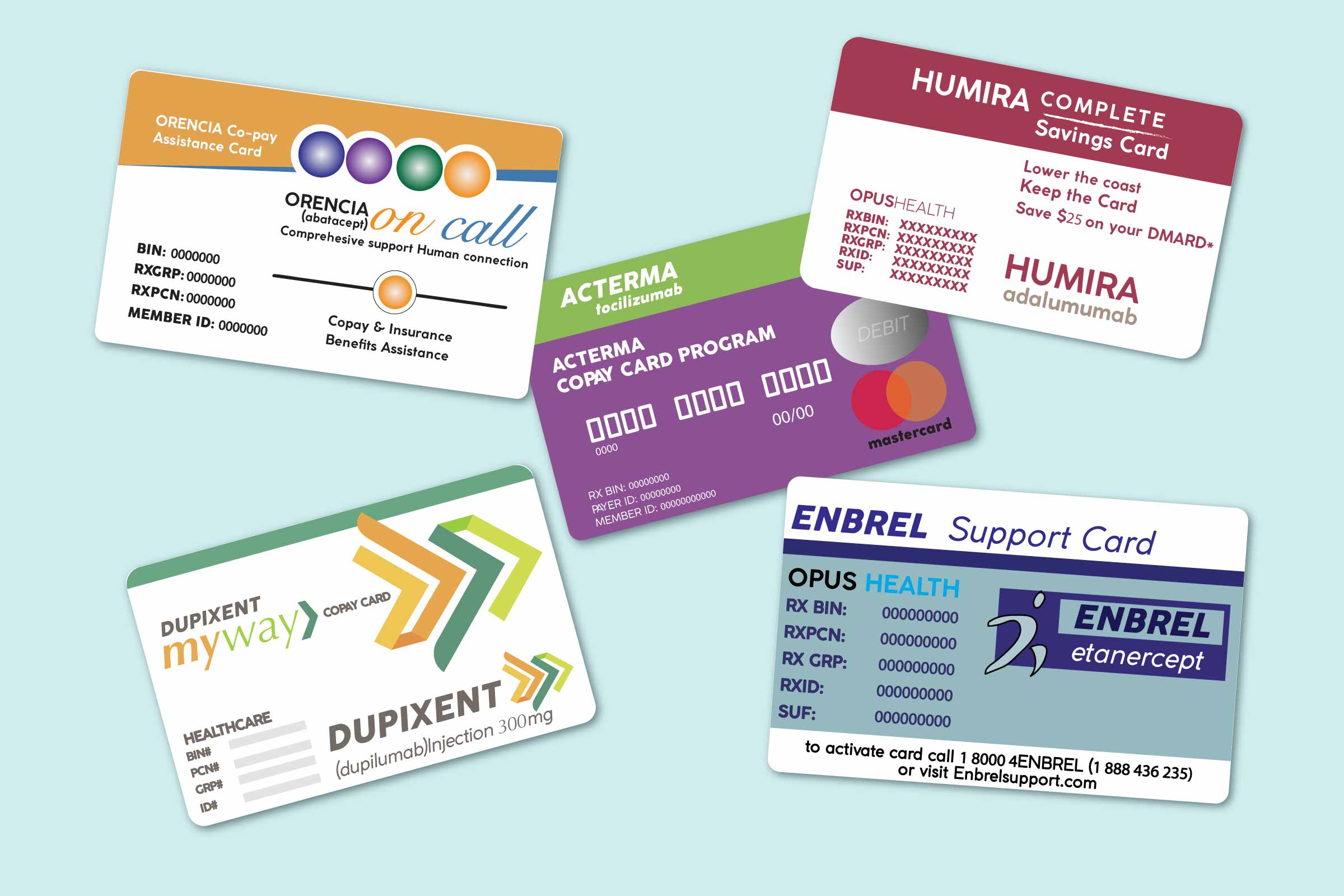
Medicaid Copays By State
Medicaid eligibility may be determined by a number of factors, and those factors may vary from state to state. The Affordable Care Act and other federal regulations have established a data-driven approach to the verification process of financial and non-financial information needed to determine eligibility. The goal has been to reduce a number of paper documents individuals are required to provide in order to determine Medicaid eligibility.
Blue Cross Blue Shield Medicare Advantage ReviewDoes Medicaid Pay For Everything
Amerigroup Medicare Advantage ReviewCo Pays For Medicaid Patients
